Dental Practitioners
How to Prevent Ransomware Attacks in Healthcare
Top 10 Strategies to Prevent Ransomware Attacks in Healthcare
- 💾 Regular Backups and Offline Storage
- Ensure frequent backups of critical data and store them offline. In the event of an attack, having accessible backups can help restore operations without paying a ransom. Make sure these backups are not connected to your main network to avoid them getting encrypted.
- 🔐 Implement Multifactor Authentication (MFA)
- MFA adds an additional layer of security, requiring more than just a password to access critical systems. This simple measure is often a game-changer in preventing unauthorised access.
- 📧 Phishing Awareness and Employee Training
- Conduct regular training to help employees identify phishing emails and suspicious links. Phishing remains the most common entry point for ransomware attacks.
- 🛡️ Keep Anti-Ransomware and Security Software Updated
- Use specialised anti-ransomware software and regularly update it to detect the latest threats. Also, ensure that all systems are patched with the latest security updates.
- 🚪 Secure Remote Access Points
- Harden your network by securing Remote Desktop Protocol (RDP) and virtual private network (VPN) connections, which are often exploited by attackers. Use strong passwords and enforce MFA for remote access.
- 🔍 Regular Vulnerability Assessments and Penetration Testing
- Conduct regular security audits to identify and fix vulnerabilities in your system. Simulate attacks through penetration testing to see how your defenses hold up.
- 🔒 Apply the Principle of Least Privilege (PoLP)
- Limit access rights for users to only what they need for their role. Segregating networks and restricting privileges reduce the impact if one system is compromised.
- 📝 Maintain a Software Inventory and Patch Management Plan
- Keep a detailed inventory of software components and ensure they’re regularly updated. Timely patching of known vulnerabilities is critical to keeping ransomware out.
- 🔌 Limit Use of Plug-Ins and Third-Party Tools
- Restrict the number of browser plug-ins and third-party applications allowed within your organization. Regularly update and monitor those that are necessary.
- 🔄 Test and Rehearse Incident Response Plans
- Regularly test your backups and run simulations of ransomware attacks. This ensures that in the event of a real incident, your team knows how to restore operations quickly and effectively.
Final Thoughts
While no single strategy can guarantee 100% security, combining these measures significantly reduces the risk of falling victim to ransomware. Staying proactive and prepared is the key to minimizing both the occurrence and impact of these increasingly aggressive attacks.
RoboDentist well and truly capable
AI-powered robot dentist performs world’s first fully automated procedure on a live human |
||
|
||
| Key Points | ||
|
||
| 🤯News – For the first time ever, an AI-powered robot played dentist and performed a procedure on a live human. While this might sound alarming, the unsupervised operation went smoothly and as planned, ending successfully without any issues. | ||
| 🦷For context – The robot, which successfully completed a crown replacement procedure on a live human in just 15 minutes—by the way, that’s eight times faster than a human specialist—was developed by the US-based company Perceptive. | ||
| 😷How it works – To perform this unique procedure, a human assistant first used a handheld 3D scanner to map the patient’s mouth. The robot then used the resulting 3D model to plan and execute the operation autonomously. | ||
| Perspective noted that the AI-powered bot performed the procedure with impressive accuracy while ensuring patient safety. The company also reported that the technique boasts a 90% accuracy rate in spotting cavities and other types of erosion. | ||
| 👨🏻⚕️From the experts – Of course, those behind the robo-dentist couldn’t help but sing its praises. | ||
| Dr. Chris Ciriello, CEO and founder of Perceptive, pointed out that this breakthrough not only makes top-notch dental care more accessible but also enhances patient experiences and clinical outcomes. | ||
| Seconding that, Karim Zaklama, a member of Perceptive’s clinical advisory board, highlighted that the AI-driven robotic system is set to revolutionize dentistry by streamlining procedures and boosting patient comfort.
Brought to you by Medinol Medical Billing Software South Africa |
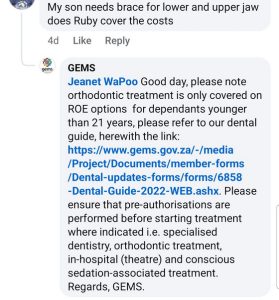
GEMS Dental Provider Guide 2024
GEMS Dental Provider Guide 2024
Rapiti Dr EV on Certificate of Need

Judge Millar’s ruling based on the certificate of need for the NHI is highly welcomed- by Dr E V Rapiti, Cape Town July 28, 2024
The Gauteng high court judgement by Judge Arthur Millar that the government’s decision to impose a certificate of need (CON) on doctors and private hospitals was deemed highly unconstitutional because it impinged on the rights of practitioners to decide where they wish to practice and would serve as a huge disincentive for investors to fund the opening of new hospitals.
Judge Millar’s judgment touched on one small aspect of the many insurmountable challenges that any government would encounter trying to set up the criteria for a doctor or health facility to apply for the certificate of need for a variety of reasons, which will be discussed in this article.
I welcome the decision not because I am opposed to equity and equality in healthcare but I am opposed to using the NHI in its contrived form as the only vehicle to achieve equity in healthcare.
As a member of the national medical and dental association of South Africa back in the 80’s, I was a keen advocate of an NHI and I, with fellow members, supported the concept to bring about equality in healthcare.
At the time the association fought vigorously against the discrimination in healthcare.
As doctors, we were not very well versed in the cost of running such a huge venture nor could we predict that most of the NHIs and NHS would fail in the advanced countries, which have far better financial and human resources than we have.
One of the major hurdles that the government faced to introduce an NHI was to find staff that were willing to work for the state because the government did not stipulate the terms and conditions of employment and their salaries.
Many doctors, over the past two decades have become extremely disgruntled about working for the state due to the unreasonable long working hours , lack of supervision and support of junior doctors, the lack of proper equipment in our hospitals, the danger to the lives of doctors and the inability of doctors to work independently because of the heavy-handed attitude of the non-medically trained managers in our state institutions on how to treat patients.
The only way that the department of health was going to staff the state hospitals back in the 90s was to introduce the CON, which would have given the government the authority to appoint doctors, wherever the state wished to appoint them.
The late minister of health, Dr Manto Tshabalala, mentioned in an interview that to develop the criteria for the CON was not easy because the problem was the detail.
In 2004 I did a great deal of research for my thesis questioning the feasibility of the CON to compel doctors to work for the state.
My conclusions after an enormous research was that the CON was a highly impractical and unworkable tool to compel doctors to work for the state without taking into account the various pros and cons of such a plan.
Some of the observations from the survey
Doctors
Almost 100% said that they will emigrate if they are forced to work in isolated areas.
The majority were concerned about the future of their children and their education.
They feared being isolated from their families.
They did not feel comfortable about losing their independence to treat their patients without bureaucratic interference.
The private sector only sees 20% of the population – highly misleading
The often used argument against the existence of the private sector is that the private sector only sees to the needs of 20% of the population whereas the state sees to the remaining 80% of the population.
This is grossly incorrect at the primary care level.
It is well established that about 50% of patients attending a doctor in the sub-economic areas and 80% in the rural areas are cash paying patients, who are seen at highly subsidised rates .
Another study has shown that the elderly visit their GP at least twice a year even if they are under the state hospital for chronic conditions.
It is at the secondary and tertiary level that only about 15% of the population seeks the services of the private specialists and private hospitals because of affordability.
Primary care options on the increase
Ever since insurance companies started offering reduced rates to cover for GPs, almost all privately employed people are able to afford GP cover, so GPs see about 50% of the patients seeking health at a primary care level.
GPs have always accounted for only 6% of the total medical aid costs, yet they play such a crucial role in the area of preventative medicine.
Many GPs have emigrated because of the total disregard for their services by funders.
Unpredictable migratory population
Ever since our independence in 1994, the South African population has become highly migratory, making it impossible to set out a fixed policy.
Due to the poor economy in the rural areas, much of the rural population has converged to the cities and peri-urban areas in search of employment and better services, so many of these rural areas have become ghost towns.
Patient survey
A patient survey revealed that 80% to 100% of patients interviewed stated that they would prefer to go to a private GP instead of going to the state.
The reasons given were distance, safety, time and convenience.
GPs were open for long hours so they could seek attention after hours and after work.
Another issue was time and safety. Given the dangers of travelling to clinics in the very early hours of the morning, patients preferred going to a GP at a time that was convenient for them.
The fact that GPs were located close to their place of residence, patients saved huge amounts of money on transport to see their GP.
GP cost
The cost of a visit to a GP was about 10 times cheaper than the state can provide for a similar service when all the indirect costs of setting up an elaborate state structure is taken into account.
Why patients choose the private sector and join medical aids
The reason that most people want to belong to a medical aid is because they want to feel reassured that in times of an emergency they will receive help immediately. Many poor households make huge sacrifices to belong to a medical aid because they are not prepared to risk their lives or that of their family by not being able to access healthcare immediately.
Currently patients with serious illnesses are not seen for up to 48 hours, patients with serious problems needing urgent surgical intervention have to wait up to a year to get an appointment.
This is the reason all politicians including our president have medical aid cover or go overseas for treatment.
Why the long wait in our hospitals
Due to poor financial resources, poor management of state hospitals and severe unearthed corruption in our state health institutions, the huge vacancies in our hospitals are frozen because the departments cannot pay their salaries.
CON – open to corruption
Given the amount of Corruption in many of our various state departments, it is not far-fetched for providers, who wish to obtain a CON in a chosen area or location they might have to pay huge bribes. What assurance can the, department of health (D O H) give the public that this type of corruption will not take place or be tightly monitored.
An example is the case of senior officials in Gauteng public works were caught in R52 million case of fraud over COVID equipment.
Why were they only caught 4 years after COVID and how many other similar cases were not traced.
CON tried in Canada
Canada tried to implement the CON in the 90s to run their NHI but the plans were shelved before it could even be submitted to parliament for debate.
We should take the lesson from Canada and shelve the Idea of using CON to force doctors to work for the state. This communistic stick method is going to leave many doctors disgruntled if they end up working for the state because they can’t find employment elsewhere.
It is the poor patients who will suffer when they are treated by disgruntled staff.
In a democracy, we should use the carrot to entice doctors to work for the state.
Based on my experience with my colleagues for over Forty years, most of them would love to see indigent patients and be part of the solution than to be looked at as the problem.
Why NHI not a suitable vehicle
The main tax base to fund the NHI would come from about 7% of the heavy tax payers.
Vat would have to be raised from 15% to 21% which is enough to cripple our economy and send millions into starvation through high food prices.
Much of our health budget is lost treating homicides, violent injuries, motor vehicle accident injuries and substance abuse related violence. The cost of these services cannot be easily calculated because it is impossible to determine the levels of crime in any. particular area due to the the sporadic nature of gang violence.
One thing that we can predict is that starvation and unemployment are closely related to the Levels of crime like rape and murder.
We rank amongst the 20 top most violent countries in the world.
For an NHI to be cost effective we need a tax base of 90%. Even in countries like the UK with high tax bases, their NHS is failing dismally. Uk doctors are leaving for Australia and our South African doctors are filling the gaps left by them.
With a 7% tax base to fund the NHI, I fail to see how our president can confidently say that the NHI will provide state of the art healthcare. He is either being purposely misleading or has his own definition of state of the art
There are better solutions to our health care problems.
The D O H must get off its high horse and stop behaving like a bunch of self-appointed dictators and engage in earnest with stakeholders from the public and private sector like every other failed state institution is doing.
Dual system necessary in a free market society
If we claim to be a democratic free market society, we have to create a space for the private sector to provide healthcare for individuals who are willing to pay for a better service.
The high standard of care in our private sector and our very competitive rates has made our country a chosen destination for people from the wealthy E U to settle in our country or to have their procedures done in our country.
This is a big money spinner for our economy and to create employment for South Africans.
It’s high time that the advisors on health policy in the D O H stop working in a vacuum to find solutions to the crisis in our health care. They have been at it for 30 years, collecting huge salaries but they haven’t moved an inch to find the Ideal solution.
To its credit, the private sector has come up with affordable medical aid packages to lesson the state load
Employers happy to fund packages
Many employers have taken advantage of the cheap packages to ensure that their staff get treatment on time to decrease absenteeism from the workplace. A healthy workforce is an important factor for our economy, which seems to have been overlooked by our. policyholder.
I sent proposals of how we should tackle our crisis in healthcare delivery about 30 years back but I have never received a response from them.
I believe that there are good workable solutions but the government needs to listen.
Our government has proved that they are incapable of running anything without running it to the ground. Eskom, water, education, railways, telecommunications, harbours and roads are the many examples that our government ran to the ground, so how can we trust them to run our healthcare without failing.
Dr E V Rapiti
Mitchells Plain
Cape Town
July 28, 2024
Dr Rapiti is a family physician working in the densely populated area of Mitchells Plain for four decades and he wrote about the CON as his thesis for his MBA in health policy in 2006.
NHI: Fear is the Enemy, Not the Patient – A Survival Guide for South Africa’s Healthcare Champions
NHI: A Sea Change, Not a Shipwreck – A Guide for South Africa’s Healthcare Heroes
Don’t let uncertainty drown your passion. Navigate the NHI waters with confidence.

The National Health Insurance (NHI) bill signing may feel like a blow, but fear not, South Africa’s healthcare professionals. Change, while often daunting, presents an opportunity to redefine your practice and future-proof your career. Let’s delve into the potential impact of NHI and equip you with the tools to navigate its various aspects.
Impact Breakdown:
- Immediate Impact: Expect adjustments to billing procedures and patient flow. Reimbursement rates and administrative burdens might shift initially.
- Medium Term Impact: As the NHI rolls out, patient demographics and practice dynamics may evolve. Collaboration with public healthcare providers might become more prevalent.
- Long Term Impact: The NHI aims to create a more accessible and equitable healthcare system. Your role in this system will be crucial in ensuring quality care for a wider population.
Gird Your Loins:
- Embrace Continuous Learning: Stay updated on NHI developments and billing changes. Invest in courses or seminars to adapt your practice.
- Network and Collaborate: Connect with colleagues and consider forming physician groups to navigate NHI collectively.
- Embrace Technology: Explore practice management software that can streamline billing and adapt to NHI requirements.
Navigating the Waters:
- Patients: Maintain open communication. Explain the potential changes to billing and waiting times. Emphasize your continued commitment to quality care.
- Funders: Stay informed about NHI payment structures and coding requirements. Work with your billing team to ensure smooth claim submissions.
- Government: Engage with healthcare authorities and professional bodies. Advocate for fair compensation and streamlined administrative processes.
Staying Sane in the Storm:
- Focus on Controllables: Channel your energy into optimizing your practice for efficiency and patient satisfaction.
- Maintain Work-Life Balance: Prioritize your well-being. Delegate tasks where possible and seek support from colleagues or mentors.
- See the Bigger Picture: Remember, you are instrumental in building a more equitable healthcare system. Your dedication is crucial for the future of South Africa’s health.
The NHI journey will undoubtedly have its challenges. However, with proactive planning and collaborative spirit, you can turn this tide into a wave of opportunity. Don’t be a passive passenger. Become a captain in navigating the NHI waters and ensure continued success for yourself, your patients, and South Africa’s healthcare landscape.
Free Medical Billing Software South Africa
Medinol Launches Medinol.Free: Free Medical Billing Software for Private Practitioners
Cape Town, 13/03/2024 – Medinol, a leading provider of medical billing software, is excited to announce the launch of Medinol.Free, a limited-time offer allowing private practitioners to access the full version of Medinol’s software for free throughout the month of March 2024.
On-prem, desktop software, Medinol.Free is specifically designed for general practitioners (GPs), dentists, and registered allied healthcare professionals operating in private practice settings. With this groundbreaking initiative, these healthcare professionals can now experience the benefits of Medinol’s advanced medical billing software without any upfront costs.
“We understand the challenges faced by private practitioners in managing their billing processes efficiently,” said Fudley Bezuidenhout Pr.Eng., Founder of Medinol. “With Medinol.Free, we aim to provide a solution that empowers healthcare professionals to streamline their billing operations and focus on delivering quality patient care.”
Key features of Medinol.Free include:
- Easy online application process.
- Self-download and install.
- Full access to Medinol’s comprehensive medical billing software.
- Easy-to-grasp self-training documentation.
- Free email and WhatsApp support for assistance with installation and any questions or issues that may arise.
“We believe that offering Medinol.Free will not only benefit individual practitioners but also contribute to the overall efficiency and effectiveness of private healthcare practices,” added Mr Bezuidenhout.
Healthcare professionals interested in taking advantage of this limited-time offer can visit Application for Medinol.Free to apply starting 15 March 2024. Don’t miss this opportunity to experience the power of Medinol’s medical billing software at no cost.
For media inquiries or further information, please contact:
Fudley Bezuidenhout
CEO, Medinol
+27 82 688 9610
info@medinol.co.za
About Medinol
Medinol is a leading provider of medical billing software solutions designed to streamline billing processes and improve practice efficiency. Trusted by healthcare professionals throughout South Africa, Medinol offers comprehensive software solutions tailored to the needs of private practitioners, clinics, and healthcare facilities. Learn more at www.medinol.co.za.
Original Press Release: